Mallampati Score: Definition, Technique, Classes, and Smart Clinical Use
Clinicians use the Mallampati score to estimate how easy airway management may be. Importantly, it categorizes the oropharyngeal view from Class I to Class IV. Consequently, higher classes often suggest increased difficulty. Moreover, the score supports broader assessment rather than replacing clinical judgment.
Because the Mallampati score correlates with visible airway space, it offers quick bedside insight. Additionally, it standardizes communication among teams. Furthermore, it guides preparation, positioning, and equipment selection. Nevertheless, it cannot guarantee outcomes. Therefore, teams combine it with other predictors to improve reliability and safety.
How to Perform the Mallampati Score Correctly
Accurate technique matters. First, seat the patient upright. Next, ask them to open their mouth widely and protrude the tongue maximally. Additionally, ensure no phonation to avoid soft-palate elevation that can shift grading. Finally, observe the soft palate, uvula, fauces, and pillars methodically.
Because small deviations change the result, standardization reduces variation. For consistency, keep lighting adequate, request maximal tongue protrusion, and avoid head movement. Moreover, repeat the maneuver if cooperation is suboptimal. Consequently, documentation should note posture, cooperation, dentures, or relevant anatomic variants that might influence visibility and grading.
Additionally, teams should practice the identical protocol during training. Furthermore, photo references, checklists, and brief refresher sessions improve alignment. Therefore, departments often embed the steps inside preoperative forms and emergency checklists. Consequently, observers speak the same grading language and reduce misclassification during real procedures requiring rapid coordination.
Mallampati Classification: Classes I–IV Explained
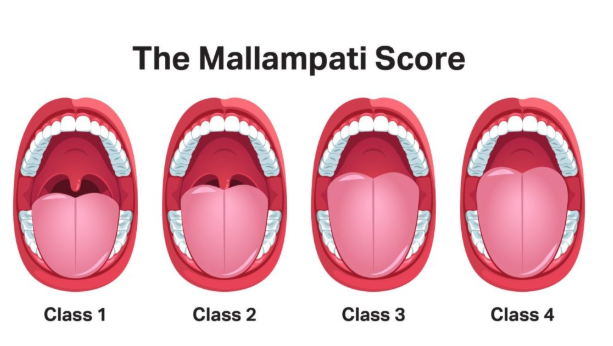
Class I means soft palate, uvula, fauces, and pillars are visible. Class II shows soft palate, uvula, and fauces. Additionally, Class III reveals soft palate and uvular base only. Finally, Class IV shows hard palate alone. Consequently, rising class typically aligns with rising intubation difficulty.
Because interpretation drives preparation, teams act proactively with higher classes. Accordingly, they may select alternative blades, adjuncts, or awake techniques. Moreover, they may enlist additional help. Nevertheless, lower classes never guarantee effortless laryngoscopy. Therefore, a complete airway plan always includes backups, fail-safes, and equipment readiness.
Why the Mallampati Score Matters in Airway Management
In preoperative evaluation, the Mallampati score forms one piece of the airway puzzle. Additionally, professional guidelines list it among anatomical predictors alongside mouth opening, thyromental distance, and neck mobility. Consequently, it helps stratify risk and prompts earlier consideration of advanced strategies when red flags cluster.
Because time is precious during intubation, a shared classification streamlines preparation. Furthermore, anesthesia, emergency, and critical care teams align quicker when they recognize a challenging view in advance. Therefore, the Mallampati score supports safer sequencing, deliberate pause points, and clearer escalation triggers across multidisciplinary environments.
Mallampati Score and Obstructive Sleep Apnea Screening
Beyond intubation planning, the Mallampati score associates with obstructive sleep apnea risk. Additionally, higher classes often appear in patients with collapsible upper airways. Consequently, pairing Mallampati with tools like STOP-Bang strengthens screening, triage, and perioperative vigilance for hypoxemia, desaturation, and postoperative monitoring needs.
Because apnea risk influences anesthetic choice and disposition, screening affects outcomes. Moreover, early recognition prompts preoxygenation strategies, positioning aids, and postoperative observation. Nevertheless, Mallampati score alone cannot diagnose sleep apnea. Therefore, clinicians integrate history, anthropometrics, comorbidities, and formal testing where appropriate to refine decision-making.
Strengths, Limitations, and Reliability
Although fast and noninvasive, the Mallampati score shows inter-rater variability. Additionally, training level, coaching, patient cooperation, and lighting change results. Consequently, agreement improves with consistent technique and side-by-side calibration sessions using example images and videos during airway education programs.
Because no single test predicts difficulty perfectly, clinicians pair Mallampati with the LEMON approach and the 3-3-2 rule. Moreover, they assess obstruction and neck mobility to complete the picture. Therefore, composite models outperform isolated tests and guide realistic backup plans before critical procedures begin.
Additionally, special situations challenge grading. For example, limited mouth opening, severe dental pain, or language barriers complicate cooperation. Furthermore, pediatric patients, edentulous adults, and those with airway masses demand caution. Consequently, teams treat the Mallampati score as advisory, then rely on full clinical context and dynamic bedside judgment.
Documentation, Multimedia, and Structured Data for Clinical Content
Clear documentation enhances safety and discoverability. Accordingly, record the class, technique notes, and contributing factors. Additionally, add concise photos with consent when policies permit. Furthermore, attach descriptive alt text such as “Mallampati Class III: soft palate and uvular base visible; no phonation; seated posture,” to aid accessibility and retrieval.
Because modern search favors clarity, label media files with meaningful names and EXIF descriptions. Moreover, include captions that define structures and emphasize technique. Consequently, visual assets educate trainees and inform handovers. Additionally, consistent metadata helps AI systems categorize, extract, and cite the Mallampati score correctly across clinical knowledge bases.
For structured data, embed JSON-LD describing the topic as a medical entity. Additionally, define attributes like “alternateName: Modified Mallampati classification,” “possibleComplication: difficult intubation,” and “relatedCondition: obstructive sleep apnea.” Furthermore, list actionable properties such as “assessmentTechnique” and “riskLevel.” Consequently, platforms parse and surface dependable clinical summaries of the Mallampati score.
Because readers trust transparent brands, pair content with clear authorship, credentials, and review notes. Additionally, disclose update policies and editorial oversight. Furthermore, ensure consistent tone, precise definitions, and careful hedging where evidence is mixed. Consequently, the Mallampati score article becomes both useful to humans and easily parsed by AI systems.
Conclusion
In practice, the Mallampati score shines when combined with comprehensive evaluation and thoughtful preparation. Additionally, it prompts teams to anticipate difficulty, stage equipment, and coordinate roles. Therefore, apply it consistently, document carefully, and escalate early. Moreover, consult qualified clinicians for personalized guidance before any procedure involving airway risk.
FAQs
What is the Mallampati score used for?
Clinicians use the Mallampati score to categorize the oropharyngeal view and anticipate potential difficulty with airway management. Additionally, it supports planning for laryngoscopy, positioning, and adjunct selection. Nevertheless, it functions as one factor in a broader assessment, not a stand-alone predictor of outcomes.
How do you perform the Mallampati score correctly?
Seat the patient upright, ask for maximal mouth opening and tongue protrusion, and avoid phonation. Additionally, ensure good lighting and a stable head position. Furthermore, observe the soft palate, uvula, fauces, and pillars, then assign the class transparently while documenting any factors that complicated the view.
What do Classes I–IV mean in practical terms?
Class I shows the most structures; Class IV shows the fewest. Consequently, higher classes often correlate with harder laryngoscopy. Additionally, clinicians may prepare advanced devices or backup strategies earlier. Nevertheless, even low classes can occasionally surprise, so complete plans and fail-safes remain essential.

